
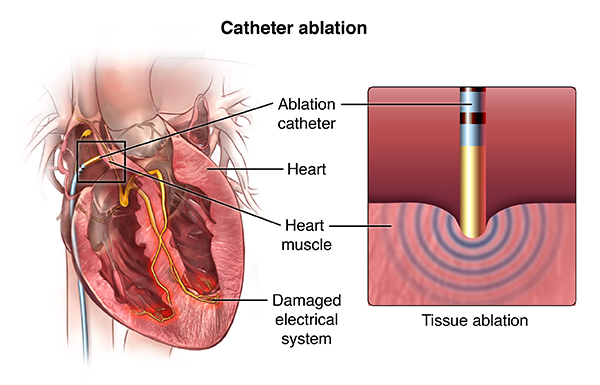
Cardiac ablation is a procedure that can correct heart rhythm problems (arrhythmias). Ablation usually uses long, flexible tubes (catheters) inserted through a vein in your groin and threaded to your heart to correct structural problems in your heart that cause an arrhythmia.
Cardiac ablation works by scarring or destroying tissue in your heart that triggers an abnormal heart rhythm. In some cases, ablation prevents abnormal electrical signals from traveling through your heart and, thus, stops the arrhythmia.
If you have been diagnosed with a heart arrhythmia-a problem with the rate or rhythm of your heartbeat-your doctor may recommend a procedure called catheter ablation to improve your condition.
Also known as a cardiac ablation or radiofrequency ablation, this procedure guides a tube into your heart to destroy small areas of heart tissue that may be causing your abnormal heartbeat.
Not everyone with a heart arrhythmia needs a catheter ablation. It's usually recommended for people with arrhythmias that can't be controlled by medication or with certain types of arrhythmia from the upper chambers of the heart. Less commonly, it may be recommended for people with arrhythmia that begins in the lower chambers of the heart.
Catheter ablation can take anywhere from 3 to 6 hours. The procedure is usually done in an electrophysiology lab or operating room where you will be monitored closely.
Before the procedure begins, you will be given intravenous medications to help you relax; some people even fall asleep. In some complex cases, you may be put to sleep by an anesthesiologist.
After the medication has taken effect, your doctor will numb an area on your arm, neck, or groin and make a small hole in your skin. Then, the doctor will guide a thin guide wire and 2 to 3 small catheters through blood vessels to your heart. In some cases, your doctor may place several catheters, which are used to help guide the procedures.
After the catheter has been placed correctly, electrodes at the end of the catheter are used to stimulate your heart and locate the problem areas that are causing the abnormal heart rhythm. Then, the doctor will use mild radiofrequency heat energy to destroy or "ablate" the problem area. This area is usually quite small, about one-fifth of an inch. Other types of ablation techniques may be used, such as cryoablation, which uses very cold temperatures to destroy the problem area. Your doctor will decide which type of ablation therapy is most appropriate for you. Once the tissue is destroyed, the abnormal electrical signals that created the arrhythmia can no longer be sent to the rest of the heart.
Most people do not feel pain during the procedure. You may sense mild discomfort in your chest. After the ablation is over, your doctor will remove the guide wire and catheter from your chest.
After the catheter ablation, you will probably need to lie still for 2 to 6 hours to decrease the risk of bleeding. Medical staff may apply pressure to the site where the catheter was inserted. Special machines will be used to monitor your heart as you recover. Some people can go home on the same day as the ablation, but others will stay in the hospital for one or more nights.
Recovery from catheter ablation is usually fairly straightforward. In the days after the procedure, you may experience mild symptoms such as an achy chest and discomfort or bruising in the area where the catheter was inserted. You might also notice skipped heartbeats or irregular heart rhythms. Most people can return to their normal activities within a few days.
Contact your doctor immediately if you have unusual pain or swelling, excessive bleeding, or consistent irregularities in your heartbeat.
Depending on the type of arrhythmia being treated, catheter ablation can have a success rate of more than 90%, but some people may need to have the procedure again or other treatments for heart arrhythmias. Your doctor may want you to remain on medications to help control your heartbeat.
After your catheter ablation, be sure to follow all instructions from your doctor, especially regarding follow-up visits, medication schedules, and safe levels of physical activity.
Online Medical Reviewer: Freeborn, Donna, PhD, CNM, FNP
Online Medical Reviewer: MMI board-certified, academically affiliated clinician
Date Last Reviewed: 2/12/2014
© 2000-2015 The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Cardiac catheterizations are typically performed on patients who experience chest pain, shortness of breath or have had a stress test that revealed a possible cardiac problem. Known as a coronary angiography, a catheterization allows interventional cardiologists to see the arteries of the heart and locate blockages. They perform the procedure by injecting a contrast dye and then inserting a catheter into an artery and threading it through the blood vessels to the heart.
In addition to using catheterizations - both radial and transfemoral - for diagnoses, cardiologists can also treat blockages at the same time. They can perform an angioplasty - inserting a small balloon to widen the artery - or implant stents, small mesh devices to keep the artery walls open.
Cardiac catheterization is performed to further evaluate coronary artery disease, valvular heart disease, congestive heart failure, and/or certain congenital (present at birth) heart conditions, such as atrial septal defect or ventricular septal defect, when other less invasive types of diagnostic tests indicate the presence of one of these conditions.
In cardiac catheterization (often called cardiac cath), a very small hollow tube, or catheter, is advanced from a blood vessel in the groin or arm through the aorta into the heart. Once the catheter is in place, several diagnostic techniques may be used. The tip of the catheter can be placed into various parts of the heart to measure the pressures within the chambers. The catheter can be advanced into the coronary arteries and a contrast dye injected into the arteries.
The use of fluoroscopy (a special type of X-ray, similar to an X-ray "movie") assists the doctor in locating any blockages in the coronary arteries as the contrast dye moves through the arteries.
Angioplasty, percutaneous coronary intervention, and stenting may be done as part of, or following, a catheterization. Fractional flow reserve is a pressure management technique that is now commonly used in catheterization to determine the severity of an artery occlusion.
An additional technique called intravascular ultrasound (IVUS), a technique that uses a computer and a transducer that sends out ultrasonic sound waves to create images of the blood vessels, may be used during a cardiac cath. The use of IVUS provides direct visualization and measurement of the inside of the blood vessels and may assist the doctor in selecting the appropriate treatment needed in each particular situation.
A small sample of heart tissue (called a biopsy) may be obtained during the procedure to be examined later under the microscope for abnormalities.
The person will remain awake during the procedure, although a small amount of sedating medication will be given prior to the procedure to ensure the patient remains comfortable during the procedure.
Other related procedures that may be used to assess the heart include resting or exercise electrocardiogram (ECG or EKG), Holter monitor, signal-averaged ECG, chest X-ray, computed tomography (CT scan) of the chest, echocardiography, electrophysiological studies, myocardial perfusion scans, radionuclide angiography, magnetic resonance imaging (MRI) of the heart, and cardiac CT scan. Please see these procedures for additional information.
A cardiac catheterization may be performed to assist in the diagnosis of the following heart conditions:
A cardiac catheterization may also be performed if you have recently had an episode(s) of one or more of the following cardiac symptoms:
If a screening examination, such as an ECG or stress test suggests a possibility of a heart condition that needs to be explored further, a cardiac cath may be ordered by your doctor.
Other reasons for a cath procedure include evaluation of myocardial perfusion (blood flow to the heart muscle) if chest pain or angina occurs after the following:
There may be other reasons for your doctor to recommend a cardiac catheterization.
Possible risks associated with cardiac catheterization include, but are not limited to, the following:
You may want to ask your doctor about the amount of radiation used during the procedure and the risks related to your particular situation. It is a good idea to keep a record of your past history of radiation exposure, such as previous scans and other types of X-rays, so that you can inform your doctor. Risks associated with radiation exposure may be related to the cumulative number of X-ray examinations and/or treatments over a long period of time.
If you are pregnant or suspect that you may be pregnant, you should notify your doctor due to risk of injury to the fetus from a cardiac catheterization. Radiation exposure during pregnancy may lead to birth defects. If you are lactating, or breastfeeding, you should notify your doctor.
There is a risk for allergic reaction to the cath dye. Patients who are allergic to or sensitive to medications, contrast dye, iodine, or latex should notify their doctor. Also, patients with kidney failure or other kidney problems should notify their doctor.
For some patients, having to lie still on the cardiac catheterization table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
A cardiac catheterization may be performed on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, a cardiac catheterization follows this process:
If the insertion site was in the arm, your arm will be kept elevated on pillows and kept straight by placing your arm in an arm guard (a plastic arm board designed to immobilize the elbow joint). In addition, a plastic band (works like a belt around the waist) may be secured around the arm near the insertion site. The band will be loosened at given intervals and removed at the appropriate time as determined by your doctor.
In the hospital
After the procedure, you may be taken to the recovery room for observation or returned to your hospital room. You will remain flat in bed for several hours after the procedure. A nurse will monitor your vital signs, the insertion site, and circulation/sensation in the affected leg or arm.
You should immediately inform your nurse if you feel any chest pain or tightness, or any other pain, as well as any feelings of warmth, bleeding, or pain at the insertion site in your leg or arm.
Bedrest may vary from two to six hours depending on your specific condition. If your physician placed a closure device, your bedrest may be of shorter duration.
In some cases, the sheath or introducer may be left in the insertion site. If so, the period of bedrest will be prolonged until the sheath is removed. After the sheath is removed, you may be given a light meal.
You may feel the urge to urinate frequently because of the effects of the contrast dye and increased fluids. You will need to use a bedpan or urinal while on bedrest so that your affected leg or arm will not be bent.
After the specified period of bed rest has been completed, you may get out of bed. The nurse will assist you the first time you get up, and will check your blood pressure while you are lying in bed, sitting, and standing. You should move slowly when getting up from the bed to avoid any dizziness from the long period of bedrest.
You may be given pain medication for pain or discomfort related to the insertion site or having to lie flat and still for a prolonged period.
You will be encouraged to drink water and other fluids to help flush the contrast dye from your body.
You may resume your usual diet after the procedure, unless your doctor decides otherwise.
When you have completed the recovery period, you may be discharged to your home unless your physician decides otherwise. Commonly, patients who undergo angioplasty or placement of a stent will spend the night in the hospital for careful observation. If this procedure was performed on an outpatient basis and a sedative was administered, you must have another person drive you home.
At home
Once at home, you should monitor the insertion site for bleeding, unusual pain, swelling, and abnormal discoloration or temperature change at or near the insertion site. A small bruise is normal. If you notice a constant or large amount of blood at the site that cannot be contained with a small dressing, notify your doctor.
If your doctor used a closure device for your insertion site, you will be given specific information regarding the type of closure device that was used and how to take care of the insertion site. There may be a small knot, or lump, under the skin at the site. This is normal. The knot should gradually disappear over a few weeks.
It will be important to keep the insertion site clean and dry. Your doctor will give you specific bathing instructions.
You may be advised not to participate in any strenuous activities for a period of time after the procedure. Your doctor will instruct you about when you can return to work and resume normal activities.
Notify your doctor to report any of the following:
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Online Medical Reviewer: Bass, Pat F. III, MD, MPH
Online Medical Reviewer: MMI board-certified, academically affiliated clinician
Date Last Reviewed: 10/31/2013
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Cardioversion is a medical procedure that restores normal heart rhythm in people who have particular types of arrhythmias. It typically involves placing electrodes on the chest that send electric shocks to the heart and is usually done as an outpatient procedure. In some cases, physicians may prescribe medications to address the arrhythmias instead of performing a procedure.
An implantable cardioverter-defibrillator (ICD) is a battery-powered device placed under the skin that continuously monitors your heart rate. It is connected to your heart with thin wires and when it detects an abnormal heart rhythm it delivers an electric shock to restore your normal heartbeat.
An implantable cardioverter defibrillator (ICD) is a small electronic device used to continuously monitor and help regulate potentially fast and life-threatening electrical problems with the heart.
The ICD, about the size of a stopwatch, is implanted under the skin just below the collarbone. It consists of a pulse generator and wires, called leads. The pulse generator contains the battery and a tiny computer. One or more lead wires connect the pulse generator to specific locations in the heart.
The ICD responds to irregular life-threatening heart rhythms from the lower chambers of the heart with either anti-tachycardia pacing (ATP) consisting of low energy impulses to promote a normal heartbeat, or shock therapy with high-energy impulses, to prevent sudden cardiac arrest. An ICD can record and store information about your heart rhythm and therapies delivered by the ICD for your doctor to review.
ATP involves rapid regular pacing impulses delivered in order to correct and restore normal rhythm by overtaking a fast irregular rhythm. Most people are unaware when this therapy is being delivered.
Defibrillation is described by many as feeling like a "kick in the chest."
The ICD can also be programmed to function as a basic pacemaker as needed. Sometimes after a shock is delivered, the heart may beat too slowly. The ICD has a "back-up" pacemaker, which can stimulate the heart to beat faster until the normal heart rhythm returns. Additionally, an ICD can act as a pacemaker not only after a shock is delivered, but also any time the heart rate drops below a preprogrammed rate.
Why might I need an implantable cardioverter defibrillator?
An ICD may be inserted in survivors of sudden cardiac arrest due to ventricular fibrillation, syncope (fainting) due to ventricular arrhythmia, or some inherited heart conditions.
It is generally inserted for those at high risk of cardiac arrest due to a ventricular arrhythmia (individuals with heart failure who have problems with the contraction of the heart, such as abnormal left ventricular ejection fraction).
There may be other reasons for your doctor to recommend an ICD insertion.
Possible risks of ICD insertion include, but are not limited to, the following:
If you are pregnant or suspect that you may be pregnant, you should tell your health care provider. If you are breastfeeding, you should notify your healthcare provider.
If you are allergic to or sensitive to medications or latex tell your doctor.
Lying still on the procedure table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
An implanted cardioverter defibrillator insertion may be done on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, an ICD insertion follows this process:
In the hospital
After the procedure, you may be taken to the recovery room for observation or returned to your hospital room. A nurse will monitor your vital signs.
You should immediately inform your nurse if you feel any chest pain or tightness, or any other pain at the incision site.
After the period of bed rest has been completed, you may get out of bed with assistance. The nurse will assist you the first time you get up, and will check your blood pressure while you are lying in bed, sitting, and standing. You should move slowly when getting up from the bed to avoid any dizziness from the period of bed rest.
You will be able to eat or drink once you are completely awake.
The insertion site may be sore or painful, and pain medication may be administered if needed.
Your doctor will visit with you in your room while you are recovering. The doctor will give you specific instructions and answer any questions you may have.
Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room or discharged to home.
If the procedure is performed on an outpatient basis, you may be allowed to leave after you have completed the recovery process. However, it is common to spend at least one night in the hospital after ICD implantation for observation.
You should arrange to have someone drive you home from the hospital following your procedure.
At home
You should be able to return to your daily routine within a few days. Your doctor will tell you if you need to take more time in returning to your normal activities. In addition, you should avoid lifting or pulling on anything for a few weeks. You may be instructed to limit movement of the arm on the side that the ICD was placed, based on your doctor's preferences.
You will most likely be able to resume your usual diet, unless your doctor instructs you differently.
It will be important to keep the insertion site clean and dry. You will be given instructions about bathing and showering.
Your doctor will give you specific instructions about driving. You will not be able to drive until your doctor gives you approval. These limitations will be explained to you, if they are applicable to your situation.
You will be given specific instructions about what to do the first time your ICD delivers a shock. For example, you may be instructed to dial 911 or go to the nearest emergency room in the event of a shock from the ICD. Calming yourself with slow deep breaths can be helpful if you are anxious after a shock.
Ask your doctor when you will be able to return to work. The nature of your occupation, your overall health status, and your progress will determine how soon you may return to work.
After implantation, your ICD will require regular evaluation or interrogation to evaluate its function and battery status, and to assess for any significant events stored by the device. Your doctor will provide details regarding recommended frequency and mode of evaluation.
Notify your doctor to report any of the following:
The following precautions should always be considered. Discuss the following in detail with your doctor, or call the company that made your device:
Online Medical Reviewer: Foster, Sara, RN, MPH
Online Medical Reviewer: newMentor board-certified, academically affiliated clinician
Date Last Reviewed: 3/27/2013
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
An electrocardiogram (ECG/EKG) is a test that measures the electrical activity of the heart. It can be used to assess for heart attacks and arrhythmias. Its results can also suggest other disorders that affect heart function.
What is an electrocardiogram?
An electrocardiogram (ECG) is one of the simplest and fastest tests used to evaluate the heart. Electrodes (small, plastic patches that stick to the skin) are placed at certain locations on the chest, arms, and legs. When the electrodes are connected to an ECG machine by lead wires, the electrical activity of the heart is measured, interpreted, and printed out. No electricity is sent into the body.
Natural electrical impulses coordinate contractions of the different parts of the heart to keep blood flowing the way it should. An ECG records these impulses to show how fast the heart is beating, the rhythm of the heart beats (steady or irregular), and the strength and timing of the electrical impulses as they move through the different parts of the heart. Changes in an ECG can be a sign of many heart-related conditions.
Some reasons for your doctor to request an electrocardiogram (ECG) include:
There may be other reasons for your doctor to recommend an ECG.
An electrocardiogram (ECG) is a quick, easy way to assess the heart's function. Risks associated with ECG are minimal and rare.
You will not feel anything during the ECG, but it may be uncomfortable when the sticky electrodes are taken off. If the electrode patches are left on too long they may cause tissue breakdown or skin irritation.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Certain factors or conditions may interfere with or affect the results of the ECG. These include, but are not limited to:
An electrocardiogram (ECG) may be done on an outpatient basis or as part of your hospital stay. Procedures may vary depending on your condition and your doctor's practices.
Generally, an ECG follows this process:
You should be able to go back to your normal diet and activities, unless your doctor tells you differently.
Generally, there is no special care after an electrocardiogram (ECG).
Tell your doctor if you develop any signs or symptoms you had prior to the ECG (for example, chest pain, shortness of breath, dizziness, or fainting).
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Online Medical Reviewer: Foster, Sara, RN, MPH
Online Medical Reviewer: newMentor board-certified, academically affiliated clinician
Date Last Reviewed: 3/3/2014
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
An echocardiogram uses sound waves to produce images of your heart. This commonly used test allows your doctor to see your heart beating and pumping blood. Your doctor can use the images from an echocardiogram to identify heart disease.
Depending on what information your doctor needs, you may have one of several types of echocardiograms. Each type of echocardiogram has few, if any, risks involved.
What is an echocardiogram?
An echocardiogram is a noninvasive (the skin is not pierced) procedure used to assess the heart's function and structures. During the procedure, a transducer (like a microphone) sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed on the chest at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the heart tissues, where the waves bounce or "echo" off of the heart structures. These sound waves are sent to a computer that can create moving images of the heart walls and valves.
An echocardiogram may utilize several special types of echocardiography, as listed below:
Other related procedures that may be used to assess the heart include resting or exercise electrocardiogram (ECG or EKG), Holter monitor, signal-averaged ECG, cardiac catheterization, chest X-ray, computed tomography (CT scan) of the chest, electrophysiological studies, magnetic resonance imaging (MRI) of the heart, myocardial perfusion scans, radionuclide angiography, and cardiac CT scan. Please see these procedures for additional information.
An echocardiogram may be performed for further evaluation of signs or symptoms that may suggest:
An echocardiogram may also be simply performed to assess the heart's overall function and general structure.
There may be other reasons for your doctor to recommend an echocardiogram.
For some patients, having to lie still on the examination table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
An echocardiogram may be performed on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, an echocardiogram follows this process:
You may resume your usual diet and activities unless your doctor advises you differently.
Generally, there is no special type of care following an echocardiogram. However, your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Online Medical Reviewer: Foster, Sara, RN, MPH
Online Medical Reviewer: newMentor board-certified, academically affiliated clinician
Date Last Reviewed: 3/3/2014
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
A nuclear stress test measures blood flow to your heart at rest and while your heart is working harder as a result of exertion or medication. The test provides images that can show areas of low blood flow through the heart and damaged heart muscle.
The test usually involves taking two sets of images of your heart — one while you're at rest and another after you heart is stressed, either by exercise or medication.
You may be given a nuclear stress test, which involves injecting a radioactive dye into your bloodstream, if your doctor suspects you have coronary artery disease or if a routine stress test didn't pinpoint the cause of symptoms such as chest pain or shortness of breath. A nuclear stress test may also be used to guide your treatment if you've been diagnosed with a heart condition.
A pacemaker insertion is the implantation of a small electronic device that is usually placed in the chest (just below the collarbone) to help regulate slow electrical problems with the heart. A pacemaker may be recommended to ensure that the heartbeat does not slow to a dangerously low rate.
What is a pacemaker insertion?
A pacemaker insertion is the implantation of a small electronic device that is usually placed in the chest (just below the collarbone) to help regulate slow electrical problems with the heart. A pacemaker may be recommended to ensure that the heartbeat does not slow to a dangerously low rate.
The heart's electrical system
The heart is basically a pump made up of muscle tissue that is stimulated by electrical currents, which normally follow a specific circuit within the heart.
This normal electrical circuit begins in the sinus or sinoatrial (SA) node, which is a small mass of specialized tissue located in the right atrium (upper chamber) of the heart. The SA node generates an electrical stimulus at 60 to 100 times per minute (for adults) under normal conditions; this electrical impulse from the SA node starts the heartbeat.
The electrical impulse travels from the SA node via the atria to the atrioventricular (AV) node in the bottom of the right atrium. From there the impulse continues down an electrical conduction pathway called the Bundle of His and then on through the "His-Purkinje" system into the ventricles (lower chambers) of the heart. When the electrical stimulus occurs it causes the muscle to contract and pump blood to the rest of the body. This process of electrical stimulation followed by muscle contraction is what makes the heart beat.
A pacemaker may be needed when problems occur with the electrical conduction system of the heart. When the timing of the electrical stimulation of the heart to the heart muscle and the subsequent response of the heart's pumping chambers is altered, a pacemaker may help.
A pacemaker is composed of three parts: a pulse generator, one or more leads, and an electrode on each lead. A pacemaker signals the heart to beat when the heartbeat is too slow or irregular.
A pulse generator is a small metal case that contains electronic circuitry with a small computer and a battery that regulate the impulses sent to the heart.
The lead (or leads) is an insulated wire that is connected to the pulse generator on one end, with the other end placed inside one of the heart's chambers. The lead is almost always placed so that it runs through a large vein in the chest leading directly to the heart. The electrode on the end of a lead touches the heart wall. The lead delivers the electrical impulses to the heart. It also senses the heart's electrical activity and relays this information back to the pulse generator. Pacemaker leads may be positioned in the atrium (upper chamber) or ventricle (lower chamber) or both, depending on the medical condition.
If the heart's rate is slower than the programmed limit, an electrical impulse is sent through the lead to the electrode and causes the heart to beat at a faster rate.
When the heart beats at a rate faster than the programmed limit, the pacemaker generally monitors the heart rate and will not pace. Modern pacemakers are programmed to work on demand only, so they do not compete with natural heartbeats. Generally, no electrical impulses will be sent to the heart unless the heart's natural rate falls below the pacemaker's lower limit.
A newer type of pacemaker, called a biventricular pacemaker, is currently used in the treatment of specific types of heart failure. Sometimes in heart failure, the two ventricles do not pump in a normal manner. Ventricular dyssynchrony is a common term used to describe this abnormal pumping pattern. When this happens, less blood is pumped by the heart. A biventricular pacemaker paces both ventricles at the same time, increasing the amount of blood pumped by the heart. This type of treatment is called cardiac resynchronization therapy or CRT.
After a pacemaker insertion, regularly scheduled appointments will be made to ensure the pacemaker is functioning properly. The doctor uses a special computer, called a programmer, to review the pacemaker's activity and adjust the settings when needed.
Other related procedures that may be used to assess the heart include resting and exercise electrocardiogram (ECG), Holter monitor, signal-averaged ECG, cardiac catheterization, chest X-ray, computed tomography (CT scan) of the chest, echocardiography, electrophysiology studies, magnetic resonance imaging (MRI) of the heart, myocardial perfusion scans, radionuclide angiography, and cardiac CT scan. Please see these procedures for additional information. Note that although an MRI is a very safe procedure, a person with a pacemaker generally should not undergo MRI, as the magnetic fields used by the MRI scanner may interfere with the pacemaker's function. Any patient with a pacemaker should always speak with his or her cardiologist before undergoing an MRI.
A pacemaker may be inserted in order to stimulate a faster heart rate when the heart is beating too slowly, and causing problems that cannot otherwise be corrected.
Problems with the heart rhythm may cause difficulties because the heart is unable to pump an adequate amount of blood to the body. If the heart rate is too slow, the blood is pumped too slowly. If the heart rate is too fast or too irregular, the heart chambers are unable to fill up with enough blood to pump out with each beat. When the body does not receive enough blood, symptoms such as fatigue, dizziness, fainting, and/or chest pain may occur.
Some examples of heart rate and rhythm problems for which a pacemaker might be inserted include:
There may be other reasons for your doctor to recommend a pacemaker insertion.
Possible risks of pacemaker include, but are not limited to, the following:
If you are pregnant or suspect that you may be pregnant, you should notify your health care provider. If you are breastfeeding, you should notify your health care provider.
Patients who are allergic to or sensitive to medications or latex should notify their doctor.
For some patients, having to lie still on the procedure table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Your doctor will explain the procedure to you and offer you the opportunity to ask any questions that you might have about the procedure:
A pacemaker may be performed on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, a pacemaker insertion follows this process:
In the hospital
After the procedure, you may be taken to the recovery room for observation or returned to your hospital room. A nurse will monitor your vital signs.
You should immediately inform your nurse if you feel any chest pain or tightness, or any other pain at the incision site.
After the period of bed rest has been completed, you may get out of bed with assistance. The nurse will assist you the first time you get up, and will check your blood pressure while you are lying in bed, sitting, and standing. You should move slowly when getting up from the bed to avoid any dizziness from the period of bedrest.
You will be able to eat or drink once you are completely awake.
The insertion site may be sore or painful. Pain medication may be administered if needed.
Your doctor will visit with you in your room while you are recovering. The doctor will give you specific instructions and answer any questions you may have.
Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room or discharged home.
If the procedure is performed on an outpatient basis, you may be allowed to leave after you have completed the recovery process. However, it is common to spend at least one night in the hospital after pacemaker implantation for observation.
You should arrange to have someone drive you home from the hospital following your procedure.
At home
You should be able to return to your daily routine within a few days. Your doctor will tell you if you will need to take more time in returning to your normal activities. You should not do any lifting or pulling on anything for a few weeks. You may be instructed to limit movement of the arm on the side that the pacemaker was placed, based on your doctor's preferences.
You will most likely be able to resume your usual diet, unless your doctor instructs you differently.
It will be important to keep the insertion site clean and dry. You will be given instructions about bathing and showering.
Your doctor will give you specific instructions about driving.
Ask your doctor when you will be able to return to work. The nature of your occupation, your overall health status, and your progress will determine how soon you may return to work.
Notify your doctor to report any of the following:
Pacemaker precautions
The following precautions should always be considered. Discuss the following in detail with your doctor, or call the company that made your device:
Online Medical Reviewer: Foster, Sara, RN, MPH
Online Medical Reviewer: newMentor board-certified, academically affiliated clinician
Date Last Reviewed: 3/27/2013
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Preventing heart disease is possible, by recognizing your symptoms and risk factors early.
Our expert cardiologists offer an integrated approach to care, including:
A transesophageal echocardiogram (TEE) is a procedure performed to evaluate your heart and the surrounding structures. The esophagus lies directly behind the heart, allowing for better quality images generally than those obtained from an echocardiogram from the chest wall. It is especially valuable in patients with valve replacements, history of a stroke, or when adequate images cannot be obtained from the chest wall.
To perform a TEE, a small flexible tube containing a small transducer is passed into the esophagus. Prior to the test, the back of your throat will be numbed first with a medication you will swallow, followed by another medication that will be sprayed into your mouth. You will then be given medication intravenously for sedation. All of this is done to make the procedure more comfortable for you.
A transesophageal echocardiogram (TEE) uses echocardiography to assess how well the heart works. During the procedure, a transducer (like a microphone) sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the heart tissues, where the waves bounce or "echo" off of the heart structures. The transducer picks up the reflected waves and sends them to a computer. The computer displays the echoes as images of the heart walls and valves.
A transesophageal echocardiogram is done by inserting a probe with a transducer down the esophagus rather than placing the transducer on the chest in a transthoracic echocardiogram.
By inserting the transducer in the esophagus, TEE provides a clearer image of the heart because the sound waves do not have to pass through skin, muscle, or bone tissue. For example, being overweight or having certain lung diseases can interfere with images of the heart when the transducer is placed on the chest wall.
Certain conditions of the heart, such as mitral valve disorders, blood clots or masses inside the heart, a tear of the lining of the aorta and artificial heart valves, are better seen with TEE.
A TEE may use one or more of several special types of echocardiography, as listed below:
Transesophageal echocardiography may be done to evaluate signs and symptoms that may suggest:
Additional reasons for which a TEE may be done include:
Possible risks associated with a transesophageal echocardiogram include:
If you have known problems of the esophagus, such as esophageal varices, esophageal obstruction, or radiation therapy to the area of the esophagus, you may not be able to have a TEE. Your doctor will evaluate you carefully before having the procedure.
If you are allergic to or sensitive to medications or latex , tell your doctor.
If you are pregnant or think you may be, tell your doctor.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
A TEE may be done on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, a TEE follows this process:
You will be moved to a recovery area, where nurses will monitor your heart rate, EKG, blood pressure, and oxygen levels.
When your gag reflex has returned, your vital signs are stable, and you are more alert, the EKG electrode pads, the oxygen probe, and the IV will be removed. You may get dressed.
You may feel weak, tired, or groggy for the rest of the day of the test. You should feel normal by the day after the procedure. Your throat may be sore for a few days after the procedure due to the insertion of the TEE probe.
If the procedure was done on an outpatient basis, you may be discharged home, unless your doctor determines that your condition requires further observation or hospital admission
If you received sedation, you will need to have someone drive you home.
You may resume your usual diet and activities unless your doctor advises you differently.
Generally, there is no special type of care following a TEE. However, your doctor may give you other instructions after the procedure, depending on your particular situation.
Online Medical Reviewer: Bass, Pat F. III, MD, MPH
Online Medical Reviewer: newMentor board-certified, academically affiliated clinician
Date Last Reviewed: 1/18/2014
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
A vascular ultrasound is the general term for a non-invasive painless test that uses high-frequency sound waves to image blood vessels including arteries and veins.
Lower extremity venous ultrasound is typically performed if a clot in the vein (deep venous thrombosis or DVT) is suspected. The veins in the legs are compressed and the blood flow is assessed to make sure the vein is not clogged. This test is also used to look for chronic venous insufficiency, or leaky valves in the veins which may cause swelling or edema.
Lower extremity arterial ultrasound may be performed in patients with peripheral artery disease (PAD), particularly for planning an endovascular procedure or surgery. It is also used after the procedure to monitor stents and grafts for signs of the blockage returning ("restenosis"). If a hematoma develops after a catheterization procedure, arterial ultrasound is also used to check the integrity of the arteries and veins in the groin.
A carotid ultrasound is a non-invasive, painless test that uses high-frequency sound waves to image the neck arteries.
Atherosclerosis may occur in the blood vessels in the neck (the "carotid arteries") which supply blood to the brain. This condition is called carotid stenosis and is typically diagnosed using carotid ultrasound. This technique allows us to look for atherosclerotic plaque and to assess whether this plaque is interfering with blood flow to the brain. As the artery narrows, the velocity of the blood flow increases; ultrasound allows us to measure the speed of the blood flow in order to estimate the degree of blockage.
Your doctor may order a carotid ultrasound if a blockage is suspected based on listening to your neck or based on your cardiovascular risk profile. This test should also be performed if you have had a stroke or a Transient Ischemic Attack (TIA).
An ultrasound of the abdominal aorta is a non-invasive, painless test that uses high-frequency sound waves to image the "aorta," the main blood vessel leading away from the heart.
When the walls of the abdominal aorta become weak, they may balloon outward If the aorta reaches over 3 centimeters in diameter, it is then called an abdominal aortic aneurysm (AAA). As the aneurysm gets larger, the risk of rupture increases.
Ultrasound imaging of the aorta is useful for measuring its size to screen for AAA. Screening is particularly recommended for men over the age of 60 who have ever smoked and for anyone with a family history of AAA. In addition to screening, ultrasound is also a useful tool after the diagnosis of AAA to monitor its size on a regular basis to see if it needs to be repaired.
Vascular studies are a noninvasive (the skin is not pierced) procedure used to assess the blood flow in arteries and veins. A transducer (like a microphone) sends out ultrasonic sound waves at a frequency too high to be heard. When the transducer is placed on the skin at certain locations and angles, the ultrasonic sound waves move through the skin and other body tissues to the blood vessels, where the waves echo off of the blood cells. The transducer picks up the reflected waves and sends them to an amplifier, which makes the ultrasonic sound waves audible.
Vascular studies can utilize one of these special types of ultrasound technology, as listed below:
Doppler ultrasound: This Doppler technique is used to measure and assess the flow of blood through the blood vessels. The amount of blood pumped with each beat is an indication of the size of a vessel's opening. Also, Doppler can detect abnormal blood flow within a vessel, which can indicate a blockage caused by a blood clot, a plaque, or inflammation.
Color Doppler: Color Doppler is an enhanced form of Doppler ultrasound technology. With color Doppler, different colors are used to designate the direction of blood flow. This simplifies the interpretation of the Doppler technique.
To assess blood flow in the limbs, pulse volume recordings (PVRs) may be performed. Blood pressure cuffs are inflated on the limb and blood pressure in the limb is measured using the Doppler transducer.
To assess the carotid arteries in the neck, a carotid duplex scan may be performed. This type of Doppler examination provides a 2-dimensional (2D) image of the arteries so that the structure of the arteries and location of an occlusion can be determined, as well as the degree of blood flow.
A carotid artery duplex scan is a type of vascular ultrasound study done to assess occlusion (blockage) or stenosis (narrowing) of the carotid arteries of the neck and/or the branches of the carotid artery. Plaque (a buildup of fatty materials), a thrombus (blood clot), and other substances in the blood stream may cause a disturbance in the blood flow through the carotid arteries.
Other related procedures that may be used to assess the heart and circulatory system include resting and exercise electrocardiogram (ECG or EKG), Holter monitor, signal-averaged ECG, cardiac catheterization, chest X-ray, computed tomography (CT scan) of the chest, electrophysiological studies, magnetic resonance imaging (MRI) of the heart, myocardial perfusion scans, radionuclide angiography, and ultrafast CT scan. Please see these procedures for additional information.
The arteries bring oxygen and other nutrients to the cells of the body. The veins take away the blood after the cells have taken in the oxygen and nutrients and given up their waste products, such as carbon dioxide. If blood flow is decreased to any part of the body, that area does not get enough oxygen and nutrients and is unable to get rid of its waste products adequately.
Decreased blood flow can occur in the arteries and veins anywhere in the body, such as the neck and brain. When the neck arteries (carotid arteries) become occluded, symptoms such as dizziness, confusion, drowsiness, headache, and/or a brief loss of ability to speak or move, may be the early warning signs of a possible stroke (brain attack). More severe symptoms, such as sudden sharp headache, loss of vision in one eye, sudden loss of ability to move arms, legs, or one side of the body, sudden forceful vomiting, or sudden decreased level of consciousness may mean that a stroke is imminent.
Some conditions which may affect blood flow include, but are not limited to, the following:
If the doctor suspects that a person may have decreased blood flow somewhere in the peripheral (arms, legs, and/or neck) circulation, vascular studies may be performed.
Evaluation of signs and symptoms which may suggest decreased blood flow in the arteries and/or veins of the neck, legs, or arms
Evaluation of previous procedures that were performed to restore blood flow to an area
Evaluation of a vascular dialysis device, such as an A-V fistula in the arm
There may be other reasons for your doctor to recommend a vascular study.
There is no radiation used and generally no discomfort from the application of the ultrasound transducer to the skin.
For some patients, having to lie still on the examination table for the length of the procedure may cause some discomfort or pain.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Certain factors or conditions may interfere with a vascular study. These factors include, but are not limited to, the following:
A vascular study may be performed on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, a vascular study follows this process:
Online Medical Reviewer: Bass, Pat F. III, MD, MPH
Online Medical Reviewer: MMI board-certified, academically affiliated clinician
Date Last Reviewed: 10/31/2013
© The StayWell Company, LLC. 780 Township Line Road, Yardley, PA 19067. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Meet Our Physicians
Stephen Angeli, MD
Gerard Eichman, MD
Tariqshah Syed, MD
David Wild, MD
Shalin P. Desai, MD
This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.
Copyright © 2026 Cardiovascular Specialists of North Jersey, All rights reserved.